“The unexpected is what makes life possible”
― The Left Hand of Darkness
Our son James has always had it hard in life. When we embarked onto the wonderful journey of bringing a baby into this world we could never imagine how hard and how profoundly our lives were going to change.
It all started with a positive pregnancy test which came to reward us, after a miscarriage a couple of years earlier due to an ectopic pregnancy, which was very disheartening for us. The positive test at age 39 was a great thing as we had been trying to conceive for about 6 months. Things were going great with growth and heart rate being in the good to excellent range. Then came week 22 and everything changed in the most shocking way.
The Unthinkable!
James’s mom felt a lump on her left breast while on a routine ultrasound test. Dr. Murillo the obstetrician at Scripps San Diego, a wonderful caring person, ordered the required tests to rule out any potential problem. Many pregnancy changes can be mistaken for false growths especially in the breast and, regarding age and risk, it was expected to be just an inflamed breast milk duct. After a breast ultrasound was inconclusive, we were recommended to wait for a month or more to see if the lump resolved itself as related to the pregnancy. Instead, to have peace of mind, we both decided to go ahead with a lump biopsy immediately.
When results came back a week later we were worried but relatively optimistic that it was just a cyst that would resolve by itself. However, the news came in and they were devastating. They showed that the lump was positive and cancer was developing. The ultrasound could not explicitly show the size or complexity of the nodule since the depth and pregnancy breast growth made it extremely hard to judge. New tests were needed and cancer specialists to be involved. Nevertheless, things were about to get more complicated.
It was week 24 of the pregnancy and now after another ultrasound at UCSD Perinatology, San Diego, which oversees high-risk pregnancies, they noticed that James’s mother had dilation in her cervix and was almost open. Now the risk of premature birth at 25 weeks was probably certain. Dr. Welkers at UCSD told us that he would be surprised if the baby could stay in utero further than week 26, as cases like ours have very slim odds at reverting the cervix changes. Now we had to deal with a new problem that endangered the baby’s life while at the same time being mostly in the dark about the cancer diagnosis.
We were prescribed progesterone suppositories to be used intravaginally in order to force the cervix to stay closed but it was a Hail Mary pass since there were only 6mm of thickness between the opening and the baby’s sack. Bed rest for the remainder of the pregnancy was also imposed. The treatment was started but just a few days later there was water everywhere and we were worried that the water had broken and the baby was coming. We ran to the hospital ER and were expecting terrible news, a baby at 25 weeks could come into this world with less than 10% chance of survival and with long term health problems in the respiratory system if he survived.
Several doctors oversaw our case during the night which measured the cervix, did not find the water to be broken, and recommended a Cerclage, which is a suture medical procedure that ties the cervix opening to force close it. Earlier that week Dr. Welkers told us that in our case a Cerclage would probably endanger both the life of the baby and mother since the Cervix seemed to be opening uncontrollably; then, if contractions started, there would need to be an emergency removal of the cerclage and /or a C section in order to resolve the situation. Several doctors did not see a clear path for a cerclage and prefered not perform it due to the immense risks associated with such close proximity to the baby’s sack.
We met Dr. Maryam Tarsa a perinatologist at UCSD at the Jacobs Medical Center in La Jolla California in the early hours of the morning after being admitted for observation. She offered the Cerclage as a possible option explaining the risks that were very likely to occur, considering the possibility of the water being broken by the cerclage needle perforating it, even causing a perforation on the baby’s skin or head. There was no guarantee of the procedure working long term but the risk of losing the baby prematurely was too great. In cases of breast cancer and pregnancy, treatment has the side effect of making it extremely difficult to conceive for several years or not at all so we saw this baby as our only chance at parenthood.
We decided to go ahead with the Cerclage procedure and the following morning preparations for the surgery started with an epidural on the spine. James’s mom was worried sick since this was her first surgery. It was not an easy pill to swallow considering what would happen after it with the variety of obstacles yet to surmount. After about three hours between prep and surgery, the Cerclage procedure was a success, there was no bleeding or perforation of the sack, and Dr. Tarsa told us that even though it was very tricky and nerve-wracking, she was able to do a near-perfect suture.
Our luck seemed to be improving that morning as now our baby had a chance at staying in the womb. The next few days were all about being in bed rest and progesterone treatment and hope that the cervix remained closed past at least 28 weeks of pregnancy to give our baby a better chance at life. Now it was time to resume cancer diagnostics while the baby was staying put.
We were referred to UCSD KOP Breast Cancer center for examination after a couple of weeks of insurance referral hell that nearly derailed our chances to treat the breast cancer at UCSD. Dr. Anne Wallace, the surgeon, and her RN Vincent Genna and their respective staff took our case and helped us tremendously with our transfer to the UCSD health system. The mammogram that was performed showed a tumor 10cm long along a duct with three different tumor growths that broke outside of the duct. Things were more serious than we could have imagined as it now was a life and death situation for mom if left untreated before James’s birth.
Second Surgery While Pregnant
That same week it was decided along with Dr. Wallace that surgery was the right course of action to remove the mass and then start chemotherapy a few weeks later to arrest any possible growth or metastatic cells that could have filtered through the lymph nodes.
James’s mom had two shots of Betamethasone administered by Dr. Tarsa’s office in order to improve our baby’s chances of survival in case breast lumpectomy surgery for the tumor triggered labor and forced the delivery. This, as it turns out, was a decision taken lightly since in all likelihood was a precursor to the chances of Autism developing in James’s young brain. In retrospect, we would probably have avoided the shots knowing the outcome now. But, at that point in time, it was an impossible situation with almost everything going against us. Hindsight is 20/20 and it is unfair to think we could have opted for no shots, considering our baby’s chances of survival by developing his lungs faster in case of preterm birth.
Surgery was performed and the tumor was extracted based on the mammogram area. An MRI could not be performed due to the negative affectation of the contrast fluid in the baby’s developing brain. As a consequence of that, pathology showed that while most of the mass was removed, positive margins were still inside the breast in some areas which means that cancer cells were still present. An MRI allows for very accurate mapping of the mass and as good as a mammogram is, it simply cannot be relied upon as a foolproof guide during surgery. The offshoot of all this means that a secondary lumpectomy surgery will be needed in the near future; however, the growth of the remaining cells would be too slow to be of consequence during the remaining three months of the baby’s gestation. All this, along with chemotherapy killing tumor cells means that cancer, for now, was stopped in its tracks as long as the treatment regimen was followed.

Chemotherapy While Pregnant
Three weeks after the lumpectomy surgery, chemotherapy with AC (Adriamycin/Cytoxan) was started while James was still in the womb during the 6th month of gestation. It was a very tough thing to see what is referred as the Red Devil (Adriamycin), be injected in huge syringes on a pre-installed arm Picc Line which delivered the deadly chemicals directly to mom’s heart as it is so corrosive that it would melt the arm if directly injected there.

With such poison, it is a remarkable miracle that the human Placenta can destroy the components of the drugs and enter the womb as deactivated substances. However, James was not immune to the treatment as the lack of vitamin supplements, lower than normal mineral levels and less than optimal conditions of the mother’s body conspired for lower than normal growth of the baby. The affectation at some point got us seriously worried after chemotherapy since James stopped kicking for several hours, we simply could not feel him. We ended up in Triage at UCSD for a checkup that gladly after careful monitoring showed that while the baby was calm, his heartbeat and vitals were within the normal range.
A total of two chemo treatments were received by James while in the womb, his mother would later receive another 6 for a total of 8 to finish treatment months later. James’s mom was extremely lucky as nausea, and other side effects of chemo seemed to be greatly reduced by the pregnancy or her own physiology which resisted the worst of the drugs without receiving much in the way of anti-nausea meds due to these being heavily detrimental to the baby so we opted not to receive them.
The only med that was taken was decadron a steroid called dexamethasone which as it turns out also increases the risk of ADHD and or Autism among other mental problems on the unborn baby. It is unclear to us if the Betamethasone shots or the decadron administered during chemo were the direct culprits of our son’s Autism symptoms but it all points out to these meds being directly connected to the outcome.
With the two chemo treatments out of the way, it was now getting closer to the 8th month or week 36 which is the timeframe selected by the Perinatologist Dr. Tarsa for delivering James as considering the postpartum treatment for cancer needed to continue as well as the cerclage risk increasing, it was the safe choice in order to avoid life-threatening complications.
As an extra complication, James’s mom was developing Cholestasis a liver disorder that can happen during pregnancy which impacts the placenta, and if the gestation continues to full term could bring life-threatening complications to the mother and child. So a premature birth was now unavoidable. It seems the chemo affected the liver and poisoned the placenta to such a degree that the body was starting to suffer the consequences. The positive thing is that after birth the condition usually reverts to normal.
James’s Birth – a real miracle fighter is born!
Week 36 arrived which was the last week of November 2018, we were admitted at UCSD Jacobs Maternity wing on the 25th, we both were in good spirits and eager to meet our little miracle baby.
Birth induction had to be performed in order for contractions to start and dilation of the cervix to happen for a natural birth. As preparation, the Cerclage knot that was installed earlier in the pregnancy was removed by the obstetrician in charge at the time, Stephen A. Hebert, MD. No problems and while a mildly uncomfortable procedure, everything came out right on that front. The cervix was now ready for opening and permitting the passage of James into the world.
After a whole day and night of induction, by noon the next day, dilation was nearing the expected 10cm needed for the baby’s head and body to pass comfortably through the vaginal canal. James’s mom was in heavy contractions by the time and needed an epidural to manage the pain which was becoming unbearable.

At about 3PM and less than 10 pushes later, James was born naturally and crying strongly onto the hands of the wonderful resident on call Dr. Erica Magelky which in her short experience had delivered over 50 babies that year. The actual labor was so fast that Dr. Hebert the Obstetrician in charge came in a minute after the birth to direct the suturing and post-birth activities.

James was a tiny baby, weighing just 2.02kg at birth or 4.45lbs, he, however, was deemed perfectly healthy and after a whole team at the NICU checked him several times, he was not interned at the Neonatal ICU or NICU for a single minute. It seems the steroids did their job and his gestation was excellent considering the circumstances even when his size was reduced due to the effects of the Chemo depleting nutrients on the body.

James was a long baby even by his diminutive size, to this day he is as tall as some 3-year-olds even when he is not yet 2. We were now ready to become parent and embrace this new miracle of life that before being born had already passed through great trials aside his mother.
James Reaches a Year of Life!
Our son was a wonderful child for most of his first year on this earth. Endless sleepless nights as with any newborn and a beautiful smile and laugh to make you forget any of the hardships that his mother was still enduring from Cancer treatment.
James’s mom was declared in remission six months after the last chemo treatment, second lumpectomy surgery, and radiation therapy were over. Mom’s hair was returning slowly but surely in a scraggly and darker tone from the flaxen blonde of before. James had always very thin lite blonde hair and almost looked bare even at six months, aside from his mom they looked like a loving team bonded by what they endured together.
James was already speaking a few words by 8 months like Mama, Dada, Yaya (Grandma), and Nam Nam which is code for I want or like a piece of food. No more words aside from sounds that seemed like words developed, he started walking and running about by year one with not a care in the world. A happy joyful and loving child that enjoyed human contact and craved hugs and being carried around in mom’s and dad’s arms. There were episodes every week or so of what could be described as colic since it was a pain emanating from the intestines that usually woke him up in the middle of the night crying and screaming. After some rocking and cradling with gentle rubs this improved and he went back to bed. This was becoming less frequent as he reached a year and now seldom happens, which seems to be related to gastrointestinal issues and not something like seizures.
Christmas came and went and James waved goodbye to his uncle who visited during the holidays, it would be the last time we would see that behavior still to this day. We were very happy at the time and saw our kid as a perfect boy with normal development and emotions, sharing his toys and food while being interested in whatever we were doing while trying to interject in conversations. By this time he was already enjoying and demanding to see the Peppa Pig Cartoon on YouTube especially at feeding time, laughed at some episodes, got euphoric on others, and even cried uncontrollably at scary dinosaurs that showed up in an episode here and there. Everything seemed normal but things were about to change completely.
13 1/2 Months and Everything Went Downhill!
By the first couple of weeks in January 2020, James was now showing some odd behavior. He first stopped saying words altogether. Then stopped looking at his grandma in the face, ignoring her and getting angsty if held by her. A couple of weeks later and he was now no longer looking or responding to his father calls, consciously avoiding looking at his face or eyes. A couple of weeks more and now his mother was the next casualty, no longer will respond to calls of his name or loud sounds to call his attention or look at his mother’s face. He also stopped being responsive when called to be carried and now it was required to fetch him every time to be held or carried, no longer looking at our activities or paying attention to us in normal ways.
At first we thought it was a phase of regression that can be common with toddlers when they learn to walk but the complete change and lack of eye contact prompted us to look for answers. The likely culprit we believed was causing this was either ADHD and or Autism presenting after the first year of life. Usually, Autism has a median age of 15 months when presenting itself in toddlers, which fits James’s timeframe perfectly. However, many autistic children never display the amount of social interaction James always showed and the need for human touch and contact. They are usually isolated and are not socially conscious of the people that surround them, they also show meltdown type behavior and problems with eye contact from very early on 6 months onward. Furthermore, both our families have no cases of Autism in the family tree that we could detect or point at. Autism in many cases has a genetic component that is inherited in families which makes it more likely to present itself in families that have members on the spectrum.
More research got us to the use of steroids, both Betamethasone and Dexamethasone used in James’s pregnancy are connected with higher indices of mental disorders including ADHD and Autism. We were now thinking that that was the cause of what we were experiencing and we felt very responsible for the fate we by our decision to use those medications as an insurance policy for his prematurity, and later on as a Cancer anti-nausea medication made our child susceptible to have a mental disorder.
Metopic Ridge Detected, Things get more complicated!
As the weeks passed and COVID-19 Virus lockdowns were happening, our child continued to withdraw from the world to the point of being sealed from whatever happened in his surroundings. No longer interacting with us as parents and or paying any attention when we tried to play with him or read him a storybook. At one point he just withdrew to corner while looking at the texture in the wall for many minutes. Our happy and loving son was no longer there or at least in a way detectable to us.
One night in despair dad saw a slanted protuberance in his frontal skull. I had seen it before but not as prominent, we did not think much of it since his family doctor never mentioned a thing about it. Looking online we were able to determine that the shape protruding from the front of his skull right between the eyes was what is referred to as a Metopic ridge. In the same vein we saw a narrowing of his forehead from above which goes further than just a ridge. Ridges are normal in many people and are usually no cause of concern. The Metopic suture in the skull can fuse anywhere from 3mo after birth to 9 months and it sometimes leaves a protuberance as fusion can be an imperfect process.
In other cases one in around 2000 in the USA, you are dealing with not just Metopic Ridge but abnormal and premature fusion of the ridge pre-birth, the condition is called Metopic Craniosynostosis and can create the following medical effects:
- The metopic suture—the joint that runs from the baby’s fontanel (the “soft spot” at the top of the head) down the forehead to the top of the nose—closes too early.
- The baby develops a noticeable ridge extending along the center of her forehead.
- The forehead will look overly narrow.
- Eyes may be spaced too closely together.
- The front of the skull may appear pointed and rather “triangular.”
In some moderate to severe cases it can cause:
- developmental delays
- learning and behavioral problems
- vision problems
- Intracranial pressure
- Hearing and Vision Impairment
Things in some even more severe instances can create brain aneurysms due to intracranial pressure and or mental retardation if left untreated. In some cases, it can also affect motor functions due to brain pressure increasing to unsafe levels. There can also be loss of life but many things have to happen including a brain hemorrhage for this to occur.
Mild Metopic Craniosynostosis and the Quest for Treatment!
We now had an idea of what was happening to James, the narrowing of the forehead was very pronounced when looked at from a top angle. If James’s Autistic like symptoms were a manifestation of crimped and underdeveloped brain frontal lobes; then Cranial Vault Remodeling Surgery or (CVR) With Frontal Orbital Band Advancement (FOA) would create enough space on our boy’s skull so that his brain would be able to develop normally after the procedure.

We got referrals from our family doctor to Neurology and Neurosurgery to get a diagnosis. These were at Rady’s Children’s Hospital in San Diego which is a world-recognized facility and one that deals with these types of cases often.
Neurology was our first appointment and it was a mixed bag, the Doctor when asked about the metopic ridge said that James couldn’t be picked out of a line-up since it was in his view a mild form of the protuberance which should not cause his behavioral problems. Then he made the case for in-hospital admittance to see why James had night episodes of pain since he was a boy. Epilepsy seizures were suspected because kids with Autistic behaviors often present epileptic seizures. We also were referred to the genetics department to rule out syndromic forms of synostosis and or something called Fragile-X Chromosome syndrome which can present Autistic like symptoms and behavioral changes. Usually not detected visually until puberty but a characteristic trait of the condition is prominent ears which James had since birth. The other characteristic is flat feet which James did not have but it could still be a positive diagnosis without that physical trait.
We did not believe James had epilepsy as we knew what seizures looked like from a pet dog with epilepsy and by looking at kids online with seizures, James never looked even close in one of his episodes, also he always touched his belly in pain when that happened at night which pointed to gastrointestinal issues which as we found out, later on, are common in Autistic children.
No Genetic Problems But The Synostosis was Increasing!
The genetic Micro Array panel and Fragile X Syndrome tests came back negative which did not show a syndromic cause for the Synostosis or behavior in James. That was great news because syndromic cases are very hard to treat and can lead to early death in many cases.
So now we had to follow up on the appointment with Neurosurgery which works on Craniosynostosis cases. We were also informed that all Synostosis cases should start at the Plastic Surgery department but the wait was so great that we opted to see Neurosurgery in the interim to have some progress on the case. COVID-19 was slowing things down so much that it was nearly impossible to advance on James’s case at an appropriate speed.
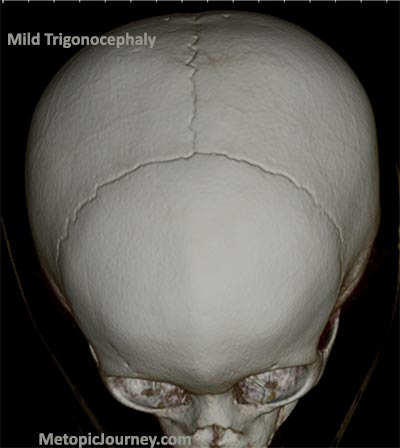
The neurosurgery appointment came and the Registered Nurse that saw us did point out the ridge but told us that our son had no Metopic Craniosynostosis Trigonocephally because his eye sockets had normal separation and he looked good and proportional. We were quite skeptical about that diagnosis since she did not have access to a CT scan or did the measurements for assessing the condition. Also, we read that night that only 15-18% of cases of Metopic Craniosynostosis present the narrowing of the eyes. That leaves out over 80% of cases that cannot be diagnosed this way. We hope she is now more informed in the ways that this condition presents itself. She however ordered a CT Scan for us to have peace of mind which was instrumental in the next phase of our saga.
James’s forehead continued to look more pointy and triangular with his behavioral symptoms increasing day by day. This was not normal and the ridge that was visible simply months back was easily seen at every angle.
CT Scan Revelations and later Confirmation!
The day for James CT Scan came and he had to be sedated, it was a very difficult day for us because it was the first time he would be apart from either of us since birth. James’s mother cried heavily as they took him to the scan in the gurney. James cried strongly after waking up from anesthesia to find that his Mother was not there and he was in a strange place. He lost his voice from the episode for a couple of days after.
The CT Scan was processed and according to the radiologist that made the diagnostic at Rady’s, James had only a metopic ridge and no evidence of craniosynostosis. This was in line with what the Neurology nurse told us and it was a big blow to our hopes since now there was no apparent answer to what James had and what affected his behavior so strongly and abruptly. We were now left with a behavioral only diagnostic which could just place James in the Autism Spectrum and not have a chance at getting any better.
This prompted us to lower our guard for a few days but then after looking at James and how he was even more inclined to withdraw from social interaction we searched for more answers and second opinions.
We contacted about a dozen doctors specializing in either neurosurgery or plastic surgery and all treated Craniosynostosis in their practices. We sent our case information and also the CT scan viewable online for them to check out. It took a bit of time for doctors to respond since they were in a once in a century pandemic and also probably in surgery most of the time. It is of note how with such a hard profession, these doctors took the time to get back to us with their thoughts and opinions. In a few cases, we either did not hear back or had a hands-off approach to the case of our son and ideally not form an opinion until he was examined in person.
A remarkable professional that helped us and continues to follow James’s case is Dr. Takeyoshi Shimoji who in Japan has operated on over 600 cases of Metopic Craniosynostosis in his remarkable career as a neurosurgeon in Okinawa. His research is extensive especially on the treatment of Mild Metopic Synostosis or Mild Trigonocephally presenting physical or behavioral symptoms. We cover his work in-depth here on the site and it should be your first stop in finding out answers. In his experience, Mild Metopic Synostosis cases tend to see remarkable benefits after surgery which are usually not operated on in many parts of the world including the American Continent. His extensive medical paper literature shows how also Autism symptoms improve after surgery especially at ages under 2.5 years old.
Other doctors that gave us their extensive knowledge are Dr. Jeffrey Fearon who runs the Craniofacial Center in Dallas Texas and has probably helped more children with Synostosis in the USA than almost any other surgeon, the last honorable mention is Dr. Jesse A. Goldstein, MD who practices pediatric plastic and craniofacial surgery at Children’s Hospital of Pittsburgh. Both of these doctors showed compassion for our case and went beyond the call of duty to give their point of view on our son’s case. They are great people and should be on your top five surgeons to consider for a craniofacial operation.
The tally of opinions on James’s CT Scan and case yielded a slight tilt towards Mild to Moderate Metopic Craniosynostosis which finally corroborated our suspicions that our son not only had the condition but time was running out to have an impact on his cognitive abilities going forward if not operated on.
James was already 18 months by now and usually, Metopic Craniosynostosis is operated on before year one in order to arrest secondary symptoms, prevent complications, and also allow for faster healing without much trauma, his time was way past the recommended age so finding a surgeon team was going to be difficult since usually the Mild Metopic Synostosis cases are rarely operated on in the US.
We were making plans to travel to Japan as Dr. Shimoji offered his help and contacts to operate on James there, though COVID-19 prevented any travel from the US to Japan, a special permit would be required with the Japanese Consulate to allow for a mercy visit to Tokyo. Other options included Massachusets and Texas as possible places that would operate on James.
Rady Children Hospital Plastic Surgery and James’s Second Chance!
Our Plastic surgery referral at Rady Children’s Hospital Division of Plastic Surgery finally came and we were prepared to make a case for surgery based on several papers by a variety of doctors and studies of post-surgery children improving mental scores after the procedure. Other papers were based on reduced cerebral blood flow in children affected by Metopic Synostosis in the frontal lobes and how after surgery this crimping of the structures in the brain permitted adequate expansion.

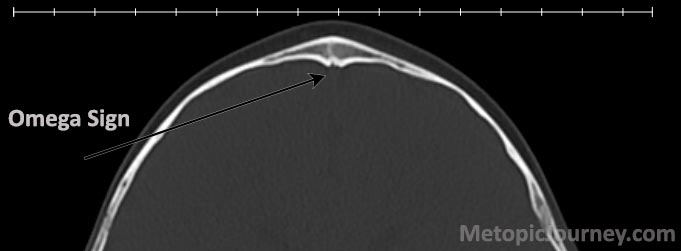
Another essential part of proving our case was our finding in the CT scan corroborated by Surgeons that James exhibited what is referred to as the Omega sign. It is an inverted U sign that forms after a prematurely fused Metopic Suture in the baby in utero and shows that the skull was already fused before birth. This was direct evidence that our son had the condition that prevented his skull from expanding properly before normal fusion of the Metopic Suture at 3-9 months of age.
Our visit was with Amanda Gosman, M.D. head of Plastic Surgery at Rady Children’s San Diego. She and her team listened to our case and explained to us the details of the procedure and also were very pressing about the risks that this type of surgery can inflict on a child, especially one that was nearing the two-year mark. Complications could include motor impairment, cognitive impairment, severe blood loss, sight loss, severe infection, brain damage, and death.
We had researched the possible complications before but our reasoning was that we as parents had to do everything in our power to help our son in any way possible to stabilize or reverse his condition. Evidence in medical journals was on our side that there is hope in cases like this and that surgery even with all the risks was essentially the only path on the table if we wanted to do something before his age and brain development was past the threshold of no return.
This decision was not made lightly on our part, we barely slept and had really entered a state of being that was unhealthy. The desperation we felt as parents, is all too familiar with kids that need medical interventions, and we can assure you that it is probably the hardest thing you could experience in life short of direct loss of a child.
Dr. Gosman and her team offered surgery as an option after our plea. We were very happy and wanted to have the operation as soon as possible so James’s age did not continue to pose an ever-increasing problem. We marked this day on our calendars as probably the most important day in our lives up to this point as it means that our boy was going to get a second chance at living a normal life.
Things were now about to become more real and the wait time eats at you every minute of every day. All we could do now is wait for the surgery and have James be healthy and strong to endure the pain and suffering to come, and hopefully come out the other side with an open future full of possibilities.
Preparing for What’s to Come!
Now that surgery for James was a palpable reality, the preparation for the big day was about to start. A surgery of this caliber is not a simple thing, the skull dome needs to be cut open in half and the whole face skin peeled down to the nose. The surgery lasts anywhere from 5 to 7 hours and there is so much blood loss that at least one transfusion is needed. As any parent in the same situation would do, we booked a San Diego Bloodbank blood draw for giving units to James. Two units were donated one from each of us parents and we directed it to the OR at the specific date.
The surgery was scheduled for August 4th, 2020 about 3 weeks from when we got the go-ahead. Every single day the actual date approached, we felt a weight on our shoulders getting heavier and a feeling of near desperation taking hold of us at times. Trying not to think about the consequences of things not going as planned we tried not to talk about it. We however cried spontaneously every few days and while we walked and played with James, we felt this awful feeling of betrayal towards him as an innocent boy. A child with no knowledge or say in what was going to happen to him. The feelings we experienced in the waiting period could drive people to deep depression and to near madness. We of course re-examined our decision many times and looking at other cases that Dr. Shimoji shared with us made it the right call over and over. We arrived at the same conclusion that doing nothing for him would negate any chance at a normal life he could have had. We had to live with our decision if things turned against us and the unthinkable happened like James being hurt, disabled, or something even worse.
Family members including James’s Grandma were there to comfort us in our time of need with encouraging words and always a shoulder to cry on and absorb our stress and pain. There is no stronger emotional pain that harming or losing a child, if that harm is caused by one’s own decisions then it becomes something even more serious as now undeniable blame is on the table. However, you cannot think like that as it is a one-way ticket to a dark place you must not visit, one with no escape. We saw the surgery on YouTube which we do not recommend to other parents as it will create imagery in your mind that you rather not have, it serves no purpose if only to know what he was going to endure and appreciate his unknowing brave act. Opting instead for giving caring love to James and dedicate every moment possible to be with him was our way to deal with the time passing.
Preparation for the surgery needed several visits to the laboratory at Rady’s for diverse blood work and a COVID-19 test for James just a couple of days prior to surgery. We also had another visit to Rady’s Neurosurgery where we now had the pleasure of meeting Michael L. Levy, M.D., Ph.D., F.A.C.S., Professor and Chief, Division of Pediatric Neurosurgery, Rady Children’s Hospital-San Diego. His demeanor from the very start was exemplary and his ear and interest for our concerns on the medical procedure of removing the Sphenoidal ridges that Dr. Shimoji in Japan recommended heavily for Autistic symptoms, made it a very important one. According to Dr. Shimoji the ridges on the Sphenoid bone below the brain are usually creating pressure on the frontal lobes in Metopic Craniosynostosis patients. By removing them then the Mirror Neuron area of the brain is free from pressure and it can freely expand.
Dr. Levy was receptive to the technique outlined in a paper by Dr. Shimoji we submitted which outlined the method and results in patients with behavioral problems. According to the studies the children had a considerable reduction in Autistic symptoms and behavior. A doctor like Levy with such an illustrious career shows just how humble a surgeon can be to the plight of concerned parents. A truly exemplary man and lucky us that he was going to be Dr. Gosman’s teammate during the surgery by cutting the bones and taking care of the brain. He explained the procedure and the risks associated including possible cuts to the Dura Matter of the brain while working on the skull dome and sphenoid. These cuts can and often happen but he assured us that closing any cuts was a routine procedure. Dr. Levy made us comfortable and gave us a sense of calm that we needed before the procedure.
James had a few more blood tests and an eye checkup with Dr. Henry OʼHalloran, M.D. Neuro-Ophthalmology, Rady Children’s who had to check him for interocular pressure which can create a situation where the optic nerve and vision might be compromised by surgery. He assured us that James was clean and ready for surgery which was another hurdle passed. The last thing was a COVID Tests two days before which came out negative, after it, we went back home to be with James and we dedicated the two remaining days to his care and making him feel good and happy. It was especially hard on the last day to hold his hand and walk around the house with him. Your thoughts trigger images of what’s to come and you try to compose yourself but it is hard. The best you can do is not think and put one foot in front of the other, detaching yourself a little from emotion helps here. Our boy had no say or choice and while our actions are geared to benefit him, we know deep down that our call has the power to harm him. It was all in god’s hands now.
Metopic Craniosynostosis Surgery!
3:00 AM on August 4th, 2020, and it’s time to wake up to get ready for surgery at 5:30AM check-in time. We had to wake up James in the middle of the night from a calm deep sleep into warmer clothes and into the car seat without him knowing why or what was going to happen. The feelings we had were of betrayal to our son for taking him there even when it was for his own good. All sorts of awful and sad things jump into your mind while you are doing it but you have to endure. It may be true that these types of operations are usually harder on the parents than the kids. Young children have a resiliency that surprises you, their pain threshold is higher so the pain is more manageable and they heal very quickly if all goes well. We were about to see it for ourselves and experience this event with all its layers including the good and the bad.
We arrived at Rady Children’s Hospital at 4:50AM and proceeded to go to the hospital entrance. James up to this point had not shown signs of being exasperated or angry from the change of schedule. He was just looking around and being interested in the new surroundings. He had been pricked several times that week for blood work so it was surprising to see how calm he was. Probably half-asleep mentally without much interest in causing a fuzz. Since COVID restrictions were in place, James’s father decided to wait outside the hospital while his Mom accompanied him to Pre-op. Needless to say, it was an extremely difficult moment for us as parents to get separated in such a trying time, but we had no choice as the guidelines are there to protect others from overcrowding. Father looked at him from outside the hospital thru a glass wall while Mom started the check-in process. After a few minutes, James and mom were ushered in and dad stayed behind. We, however, were happy that the day had come in that he will now get the much-needed operation and his mental prison could with some luck be ended.
James’s mom got to speak with both Dr. Gosman and Dr. Levy before the surgery and gave them letters to each which expressed our sincere thanks and reminded the team of the sphenoid bone ridge removal technique that Dr. Shimoji had been so adamant about for our son. Both were calming and reassuring as they got ready for entering the OR area and scrubbing. James’s mom was able to stay with him up until the moment they took him to anesthesia at which point she started to sob and the psychological rollercoaster of up to 7 hours of wait time was about to start. James was well composed and was calm and sleepy as they took him in. Nothing can really prepare you for a moment where your only baby son is taken to an operating room for an operation that is not just serious but risky. It doesn’t matter how much you think you have prepared for this moment, a huge space in our hearts had been removed and pulled away at our own behest. Now we had to pray and wait for news about how everything was progressing.
The Cranial Vault Remodeling with Frontal Orbital Advancement Surgery or CVR FOA started at about 7AM at Radys Children’s Hospital, and we got the first update at about 10 AM when Dr. Levy who was first in line for the surgery and did all the bone cutting and at our request the Sphenoid ridge shaving, which was recommended by Dr. Shimoji in Japan to help with Autistic Symptoms by relieving pressure under the frontal lobes. Dr. Levy talked calmly and explained that everything was going nicely with no complications and that they did everything they could to give enough space to the frontal lobes before Dr. Gosman started the cranial vault remodeling.
James’s bleeding was also under control and everything was going well. We were relieved but still only halfway to the end of the procedure. There was a transfusion happening due to blood loss as expected and they used one of our donated blood units, we still do not know if it was Mom’s or Dad’s blood that was used. Maybe it is best not to know, as we can just know it could be any one of us that now shared part of our body with him.
Dr. Gosman was working now on reshaping our boy’s skull by creating a 3D Puzzle to make an aesthetic and pleasing forehead shape derived from the bone fragments that were cut out and divided from his Metopic Cranium shape. To this day we are marveled at the shape of James’s skull and how Dr. Gosman was able to create a perfectly shaped frontal bone shape with minimal holes in between the fragments. Her skill is really a cut above what we could have expected.
We as parents were praying to God that our boy was doing fine and that his pain and suffering were manageable. Every minute felt like an hour and every hour like a day. We tried to sleep some because of not doing so for about 27hrs but our bodies would not let us do it, our baby was in a battle and we needed to be ready for him. At the same time the operation was happening, an enormous explosion in Beirut Lebanon happened which would make this day even more memorable as at first it was thought of as a nuclear explosion. It turned out to be thousands of tons of fertilizer and fireworks blowing up and it was pure negligence in the part of the government there. This day would be easy to recall because of this fact. Family and friends were also listening to updates on our boy’s surgery and prayers sent our way. Even a Reiki circle was formed in California to send good energy to our baby. Thank you all!

At about 1PM the surgery was over and James was taken to the Post-Op recovery area. His mom was at his side and described to dad how he looked and what was happening. His tiny head was now covered like a mummy in bandages and a tube was coming out behind his right ear which was placed as to drain fluids like lymph and blood that were oozing from inside the skull. The swelling seemed to be prominent but he looked peaceful and very tired. The nurses explained that the swelling will be increased heavily by the 3rd day and then it should start to go down. Frontal orbital advancement requires a cut of the eyebrow bone band to be moved forward in order to estimate skull growth in time. The surgeons overcompensate the skull shape and size in order for the head to continue growing years later until adulthood. By year 5 the brain gets to 90% size and by 25 it stops growing. Head shape and size usually stabilizes by age 22.

Post-Op and The Days After!
James was hurting as the swelling was very pronounced. His head was bandaged completely like a mummy and his eyes all purple and shot tried to open to no avail. The surgeons assured us everything went very well and that no excessive blood loss had occurred. He had a catheter for urine installed and a drainage tube from behind the ear draining excess fluids. He was calm and cried very little the first day, he was comforted that mommy’s voice was beside him and his hand being held. We cannot imagine what he was feeling at the time disoriented and banged up. His courage was heartwarming and so admirable that it made us appreciate his situation even more.
He could barely retain any liquids in his mouth and was in pain even from sucking on his milk bottle filled with Gatorade and water. It was too soon for him to be held but talking to him and caressing his arms and hands seemed to calm him. He was on antibiotics to prevent infection and moving from morphine pain killers to Tylenol and ibuprofen. Every 3 to four hours a pain killer was given by mouth and fluids administered intravenously during day and night.
By day two post-op his eyes were starting to swell more and more and his face now looked like a badly beaten boxer after a prizefighter. Dr. Gosman’s team came in and removed James’s head bandage during the first hours in the morning. His head slowly uncovering revealed a scar waving from ear to ear with sixty massive stitches. The scar is cut in an up and down wave or semi-circle pattern to allow for hair growth to occur later and cover the scar more easily. The swelling was massive but expected, the head had swelled so much it looked at least 40% bigger than usual and his entire forehead felt squishy filled with water and or lymph fluids. The drain was working but it would take many weeks for the swelling to completely disappear.

James’s eyes remained closed from the swelling and his painful cry during night and day got him very tired. He slept a lot but was eager to start drinking some milk from his bottle and some soft puree food. The hospital had changed COVID 19 restrictions and allowed for us both parents to spend the night at his side which was good as he needed constant attention and we both needed some sleep.

Mom heard a soft sound that sounded like Mama and she started crying in joy. James had lost all the small word vocabulary he had learned by age 13 and 1/2 months and we had not heard anything until now. If it was a wishful reinterpretation that could have been so, but it was enough for us to be encouraged that the operation was creating changes in his brain already.

Day 3 came and James was eating and drinking easier with less trouble swallowing and he was permitted to be carried by mom and dad as the urine catheter was removed and no longer needed. No sign of infection was present and we were told he could be allowed to be checked out of the hospital that afternoon. His drainage was removed and we were coached on how to clean his scar wound twice a day for a few weeks. James was still not able to open his eyes and the swelling was massive, his eyes had ballooned to twice the volume at least from the outside but it was also normal we were told.

At about 1PM on the third day after the operation, we were checked out of the hospital and we were heading to the car. The parking lot was about a block away and James was moving his head left and right using his ears to perceive the world as his eyes were not useful at the time. He seemed happy and content to be out of the hospital and listening to us talk. The most remarkable moment came when we sat him on his infant car seat. Being blinded he was clinging to our clothing and then touched all around his chair and the car and remembered it so vividly that he became instantly calm and happy even showing a little smile. For a 20mo old baby, it really made us feel that he was stronger than we could have possibly imagined by adapting to the situation.
Once at home he felt calm and rarely cried, he was able to open one of his eyes a fourth of the way which let him see his room, us, and his home. He was relieved and wanted to eat a lot and then sleep. For the entire week after, we were on a regimen of Tylenol and Advil for toddlers every 5 hours or so to control pain. He was doing well and at his follow up check-up with the nurse at the hospital was given good recovery marks and on track for getting back to normal.
His eyes were fully open by day 7 after the operation and he felt so good that he wanted to walk around the house, assisted by us as to not bump his head. It was notable at this time that James was showing some signs of improvement cognitively as he started to look at us in the eyes sporadically. A couple of more visits were done at the surgeon’s office to check his stitches and swelling, everything was progressing nicely. His wound was cleaned for 4 weeks with 50% hydrogen peroxide and finished with a coat of Aquaphor cream twice daily by us as to keep it clean and uninfected. We also were able to give him a bath which he did not like as his head was still hurting and the wound tender. It is of note that he has never liked to be sprayed with water on the head.
The operation and recovery had progressed better than we had hoped and by the first month he seemed very normal, swelling was still present but largely reduced which started to expose the plates that were screwed in place to hold the new skull bone structure. These plates are made of biodegradable material and will last about two years until they are consumed by the immune system, the same goes for the screws. By that time his skull should have fused together for the most part and any holes between the bone fragments permanently closed.
With most of the danger out of the way, it was time to start therapy for James and improve his cognitive skills and well as check his motor coordination which was a little behind due to his condition. Two months and a 1/2 after surgery, James started OT or Occupational therapy, physical therapy, and speech therapy. But before that, we did our best to teach him new things and get him to engage more with faces and do new things that before were impossible to try due to his lack of concentration.
We saw remarkable improvements after the surgery until right before therapy started, our boy is now able to look at our faces constantly, he has regained the ability to say Mama and Dada sometimes, he has completed puzzles intended for his age group as well as complete many that are geared for older children. His motor skills have improved greatly and while he is still behind the curve, he should be able to catch up to a kid his age in about a year with therapy. James is much happier and present socially, craves human contact, and is very aware of what happens in a room including being aware of people entering or leaving the room. He has run to his parent’s arms when called and uncalled and is able to concentrate heavily on doing things. We are encouraged greatly by his progress and hope to one day have a kid that can blend into the world with social and physical skills that are normal for his age. His Autistic traits continue to show but less and less as the weeks pass, with some luck he could outgrow them and jump out of the spectrum or at least be able to lead a normal life.
We feel the Mild Metopic Craniosynostosis operation gave our son a second chance at life and turned what could have been a depressing and grim future into a full life experience waiting to be explored. We thank Dr. Gosman, Dr. Levy, and Dr; Shimoji for their incredible contributions to our son’s life. Their dedication to the well being of others above their own is an example for us all!
Our son will continue to be followed as he grows and this progress will be posted on MetopicJourney.com for you to read over the years. His developmental milestones are logged here and we are happy to respond to your questions as time permits.
Thank you for reading our son’s story!
Parents of James!
The Story Continues:
-You can read on James’s progress after the operation at his developmental-log here!